Published on: July 23, 2025
Author: Admin
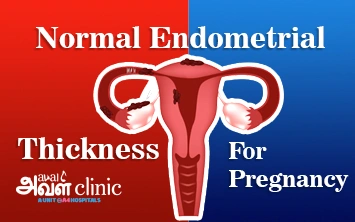
Endometrial thickness plays a major role when it comes to achieving a healthy and successful pregnancy.
Not having the ideal thickness of the endometrium can lead to early miscarriage or implantation failure. The ideal uterine lining (endometrial lining) for a healthy pregnancy should neither be extremely thick nor extremely thin.
According to the WHO (World Health Organisation), the normal endometrial thickness for pregnancy is 7-14 mm. They also state that women over 190 million worldwide have abnormal endometrial thickness, which is a manageable disorder. However, early diagnosis and appropriate treatment are essential to prevent the severe complications related to conception.
This blog helps you understand the potential symptoms, optimal measurements of endometrial thickness for pregnancy, factors that influence the condition, and available treatment options to lead a better life.
Normal Endometrial Thickness in MM at Different Stages
The inner layer of the uterus is commonly referred to as the endometrium. A healthy endometrium is essential to maintain a healthy reproductive system in women. The thickness of the endometrial tissue is largely influenced by hormones like estrogen and progesterone, cyclically. Endometrium, in general, delivers the nutrients that are essential to prepare the uterus for both pregnancy and the menstrual cycle.
If the implantation occurs, the endometrium produces a supportive atmosphere by becoming thicker to nourish the growing embryo. If the implantation doesn’t occur, the endometrium starts to shed the uterine lining, becoming thinner.
It is generally a cycling process which happens throughout the reproductive life of a woman. The thickness of the endometrium could be significantly different for a young girl before she attains puberty. However, the normal endometrial thickness of women in their reproductive age in mm is:
Menstrual cycle
During the menstrual cycle, the uterine lining tissue becomes thin because of the shedding process. The measurement could vary anywhere from 2 to 4 mm at this stage.
Follicular phase
The days following menstruation are referred to as the follicular phase, specifically until the day of ovulation. At this phase, the uterine lining tissue starts to grow from a thin layer of 2-4 mm to 5-7 mm thickness. This significantly happens due to the increasing estrogen hormones.
Luteal phase
The days following ovulation are referred to as the luteal phase, specifically until the menstrual cycle or pregnancy. At this phase, the uterine lining tissue reaches its utmost thickness, varying anywhere between 7 and 14 mm. Many experts consider this range of thickness to be normal and ideal for pregnancy.
IVF Success
The ideal thickness of the endometrial tissue for IVF success is anywhere between 8 and 14 mm. While some studies suggest that the endometrial thickness of above 10 -15 can deliver higher live birth rates.
Postmenopausal phase
The months following the last menstrual cycle of a woman are referred to as the postmenopausal phase. During this phase, the endometrium reaches its thinnest, typically below 5 mm.
Symptoms of Abnormal Endometrial Thickness
Even though the endometrial tissue is involved in the natural cycling process of women’s reproductive health, both excessive thickening and thinning can lead to several issues. Some of them are:
- Noticing bleeding even after menopause.
- Noticing menstrual bleeding in between cycles.
- Heavy bleeding during the menstrual cycle.
- Prolonged bleeding during the menstrual cycle.
- Abnormal menstrual cycle. Typically, shorter than 21 days or longer than 35 days.
- The absence of menstrual bleeding (amenorrhea).
Factors Influencing the Endometrial Thickness
The following are some of the detailed factors that are most often associated with influencing the endometrial thickness:
Hormonal Fluctuations
Fluctuations in hormone production, particularly estrogen and progesterone, are the significant influencing factors of endometrial thickness. Estrogen hormones are responsible for thickening and growing the endometrial tissue. Progesterone hormones are responsible for preparing the endometrium for potential implantation. Fluctuation in the production of any of these hormones can potentially lead to abnormal growth of the uterine lining (endometrial hyperplasia) or other abnormalities in the uterus.
Menstrual Cycle Phases
The layer of the endometrium may certainly vary in its thickness throughout the menstrual cycle of women. It may increase its thickness during the follicular and luteal phases, and decrease during the menstrual cycle. This is because of hormonal fluctuations, especially estrogen and progesterone, which play a key role in regulating the endometrium.
Age
With increasing age, particularly after 40 years, the thickness of the endometrium typically decreases. This is primarily because of the reduced estrogen levels and endometrial atrophy.
Medical Conditions
Medical conditions like PCOS (polycystic ovary syndrome), endometrial polyps, fibroids, and endometriosis can contribute to the development of abnormal endometrial thickness (endometrial hyperplasia) or other irregularities in the uterus. This is because these conditions can stimulate hormone fluctuations, which hugely influence the changes in the endometrial lining.
Medications and Hormone Therapies
Medications and hormone therapies play a significant role in influencing the endometrial thickness. Estrogen hormones are responsible for thickening and growing the endometrial tissue. Progesterone hormones are responsible for preparing the endometrium for potential implantation. Medications used in treatments for breast cancer can increase the estrogen levels. This may lead to the endometrial thickness. Conversely, certain medications that reduce estrogen or therapies that increase progesterone can result in a thinner endometrium.
Lifestyle Factors
Unhealthy lifestyle habits like stress, lack of exercise, poor diet, and being obese can cause thickness in the endometrium. All of which can lead to hormonal imbalance, particularly excess estrogen. This can largely stimulate the unnecessary growth of endometrial tissue.
Fertility Treatments
Fertility treatments like IVF can influence the endometrial thickness. The ideal thickness of the endometrial tissue for IVF success is anywhere between 8 and 14 mm. To achieve this, your healthcare provider may prescribe certain hormonal medications that can stimulate the production of more estrogen hormones. This may ultimately lead to thickening of the endometrium, which is good for the process.
Treatments for Abnormal Endometrial Thickness
The fertility condition associated with endometrial tissues can happen either because of thinning or thickening of the uterine lining. Both of which can significantly impact menstruation, pregnancy, and fertility. Endometrial thinning can most often result in early miscarriage or implantation failure. While endometrial thickness can result in infertility. It is also associated with conditions like PCOS, hyperplasia, and polyps. However, experts say that the condition can be managed if diagnosed early, along with appropriate treatments. Listed below are some of the treatment options for abnormal changes in endometrial tissues. They are:
Treatments for Thin Endometrium
1. Estrogen Therapy
Estrogen therapy is most often used during IVF (in vitro fertilisation) treatments. The therapy involves stimulating the estrogen production through which the endometrium’s growth is improved. Estrogen therapy can be recommended in the form of injections, patches, or pills. Your healthcare provider may prescribe the form of medication based on the patient’s tolerance and its effectiveness on them. Meanwhile, your healthcare provider may also suggest taking progestin supplements along with it. This is because prolonged exposure towards unopposed estrogen can have negative impacts on health. It may include hyperplasia or endometrial cancer. To minimise the impact, progestin supplements are typically prescribed.
2. Platelet-Rich Plasma (PRP) Therapy
Platelet-Rich Plasma (PRP) therapy is performed by utilising the growth factors and cytokines that are found within the individual’s platelets. This may certainly help with stimulating anti-inflammatory properties, angiogenesis (formation of new blood vessels from the existing ones), and cell proliferation (formation and division of cells) within the uterus. These are essential to maintain a healthy endometrium. In addition, PRP can also help with promoting endometrial tissue adhesion and migration. All of which can lead to thickening and improve the receptivity of the uterine lining.
3. Hysteroscopy
Hysteroscopy is a diagnostic procedure. It is used to examine the uterine cavity by visualising it simultaneously. The procedure is often used to determine the thickness of the endometrial tissue, especially in cases like endometrial abnormalities or abnormal uterine bleeding (AUB).
4. Medications
Medications like low-dose aspirin, sildenafil (Viagra), hormonal therapies like estrogen and progestogens, and L-arginine can help repair endometrial tissues and their growth. These medications, along with vasodilators, play a key role in improving the blood circulation to the uterus. Thus, helping to improve endometrial thickness.
5. Lifestyle Modifications
Along with the medication, your healthcare provider may also suggest leading a healthy lifestyle, which can positively impact the health of the endometrium. Including a balanced diet, reducing stress, exercising regularly, and quitting smoking and drinking can all help improve the endometrial thickness.
Need expert advice? Consult our doctors now!
Call Now: 80047 80048Treatments for Thick Endometrium
1. Progestin Therapy
Progestin therapy is often associated with balancing estrogen hormones. By doing this, it can counteract the effects of estrogen on the growth of endometrial tissue. Along with it, the progestin therapy helps control endometrial hyperplasia by promoting cell maturation (decidualization).
2. Surgical Removal of Tissues
1. Hysterectomy
Hysterectomy is the removal of the uterus. It is widely considered the last line of treatment for endometrial thickness. Your healthcare provider may suggest the option if they suspect the condition leading to endometrial cancer. The procedure is generally associated with quicker recovery and less pain, if done laparoscopically.
2. Hysteroscopy
Hysteroscopy is a diagnostic procedure. Sometimes, it is used to treat conditions related to endometrial thickness. The procedure is made to examine the uterine cavity by visualising it simultaneously. It is often used to determine the thickness of the endometrial tissue, especially in cases like endometrial abnormalities or abnormal uterine bleeding (AUB). If the uterine lining is diagnosed with too much thickness, a biopsy may be recommended to rule out the presence of cancer cells in the endometrium or hyperplasia.
3. Dilation and Curettage (D&C)
A Dilation and Curettage (D&C) is a procedure that is used to treat as well as diagnose the abnormalities present in the uterus, especially the uterine lining. The procedure involves scraping the abnormal growth of tissues within the endometrium. It can also be used to treat (scrap) conditions like polyps, fibroids, abnormal uterine bleeding (AUB), and hyperplasia.
4. Endometrial Ablation
Endometrial ablation is a procedure that is often associated with regulating heavy menstrual bleeding. This is done by removing or destroying the thickened endometrial tissue within the uterus. The treatment is often suggested when other methods have failed to regulate the heavy menstrual bleeding.
3. Medications
Medications like letrozole and anastrozole can help minimise the growth of endometrial tissue, especially in cases like endometrial hyperplasia. This is because these medications play a role in regulating the production of the estrogen hormone, which is the key contributor to endometrial thickness.
4. Lifestyle Modifications
Along with the medication, your healthcare provider may also suggest leading a healthy lifestyle, which can positively impact the health of the endometrium. Including a balanced diet, reducing stress, exercising regularly, and quitting smoking and drinking can all help with regulating the endometrial thickness.
Summary
A healthy endometrium can be an indicator of a healthy reproductive system in women. When it comes to fertility, especially treatments like IVF, the endometrium plays a significant role. However, the thickness of the endometrium alone is not the only contributor to successful implantation. Factors like endometrial pattern and receptivity also play a role in the implantation process.
You need not worry about any abnormalities in the uterine cavity. Having a consultation with specialists like Aval Clinics can largely help with treating the condition in a more effective way that can bring a healthy difference in your reproductive life.